
The role of the VHA in driving successful digital innovation
Learnings from the largest integrated healthcare system in the US
Innovative technologies and digital health solutions offer enormous possibilities to support sweeping improvements in the safety, effectiveness, and equity of Veteran care across the nation. From preventing diabetic limb loss to helping visually impaired Veterans live safer and more independent lives, digital health has the potential to improve the lives of every Veteran, everywhere. However, without a framework for operationalizing and scaling innovation, this potential is not fully realized in any major healthcare system.
One of the reasons is that digital health technologies are not a silver bullet. More technology, more data, and more widgets in our toolbox does not lead to a transformation. Rather, quality health, expanding access, improved equity, and system efficiencies are driving successful and meaningful change in the lives of Veterans and those who care for them. While the terms “innovation” and “digital health” aren’t new to our lexicon, there are important questions we must ask when we combine the two:
- How do we make sure we use digital health to deliver the right care at the right place at the right time and not just start data mining?
- How can we ratify that the new digital tools in the healthcare toolbox minimizes health and access disparities, and not exacerbate the digital divide?
- How do we ensure that we use digital innovation to streamline clinical workflows and reduce administrative burden for clinical teams — not add layers of inefficiency and frustration?
On June 16, 2021, the Veteran’s Health Administration (VHA), in partnership with the Digital Medicine Society (DiMe), hosted the inaugural Digital Health Symposium, “Evaluating and Adopting Digital Health Technologies for Veteran-centered Care”. The symposium convened Veteran patient voices alongside VHA leadership and both clinical and Veteran innovators from different offices and across the country.
Digital Health Stories in Action
Innovators showcased seven extraordinary examples of digital health innovation in VHA practice — highlighting the impetus for innovation grounded in Veteran need, describing the challenges along the way, and the strategies that drove success. Let’s take a look:
- Smart White Cane: Brian Higgins, a Veteran and blind rehab specialist (pictured below sharing his story) developed Smart White Cane with sensor technology to aid navigation for blind and visually impaired Veterans
- SmartMats: To end diabetic limb amputation at VHA, foot thermal imaging via SmartMats are helping early detection of diabetic foot ulcers and dropping hospitalizations by 92%
- SmartHEART: Smartphone technologies and home-based rehabilitation are providing virtual-cardiac rehabilitation capabilities improve Veteran’s heart health
- SCI/D remote monitoring: Improving Veteran’s quality of life by coordinated service using innovative digital tools and remote capabilities is helping protect Veterans with spinal cord injuries/disorder (SCI/D)
- VEText: With more connectedness, zip codes no longer define access to healthcare. The VEText program aims to address the 9 million appointment no-shows a year
- TeleSleep: Comprehensive Sleep Telemedicine program is expanding national access and sleep for Veterans, especially in rural or remote regions of the country
- ERTHI: Better hearing aids are manifested virtually for Veterans by the Enterprise Remote Tuning of Hearing Instruments (ERTHI)
Brian Higgins, a Veteran and blind rehab specialist at the VA Palo Alto’s Western Blind Rehab Center, shares his innovation story on developing “The Smart White Cane” using sensor technology to help blind and visually impaired Veterans to navigate safely.
These powerful solutions taught us that the innovation process is not a one-stop-shop. The VHA is the largest, integrated healthcare system in the U.S. It is a complex federal healthcare system where barriers to innovation are perceived as higher than in the private sector. There is a need for a robust foundation and an intentional approach — to develop and deploy the digital health solutions that are accessible, effective, efficient, and equitable. As the U.S. healthcare system envisions to build innovative health solutions using the emerging digital tools, all stakeholders in healthcare innovation are responsible for implementing the following learnings from the symposium:
- Early engagement of key stakeholders (Veterans, clinicians, etc.) is critical for digital health innovation
- Most innovations don’t succeed in isolation
- Operationalizing radical innovation requires a well-designed plan
- Treat innovation as a marathon, not as a sprint
- Technology doesn’t discriminate — and neither should our innovations
1. Early engagement of key stakeholders (Veterans, clinicians, etc.) is critical for digital health innovation. Engaging Veterans and clinicians early on and at every step of the innovation was common to all successful innovations. We need to take a “yes, and…” approach, combining both Veteran-centric and clinician-centric strategies as we design, develop, and deploy digital health technologies across the health system.
2. Most innovations don’t succeed in isolation. Siloed work stifles progress and a disconnected system may do more harm than good. The success of digital health innovation requires deep collaboration across clinical, technical, and Veteran experts. Multi-stakeholder and inter-office collaboration are foundational success factors for advancing most innovations. As we build our digital solutions, a balanced mix of aligned values, clarity of desired outcomes, and collaborative involvement can lift all boats across the entire innovation ecosystem.
3. Operationalizing radical innovation requires a well-designed plan. While almost every organization has dreamt of radicalizing innovation to transform their entire system, disrupting the status quo is full of challenges, especially for an enterprise as complex as VHA. Aspects like the organizational readiness and infrastructure for innovation, innovation-enabling culture and management, and system-wide strategic roadmap of success are key components to drive successful and sustainable outcomes at scale.
As we start operationalizing digital health innovation that drives meaningful change, we need to start asking this question, again and again, “How can we deliver the most innovative solutions that serve the most people?”
The answer starts with: 1) creating a framework for shared value measurement for innovations; 2) establishing technical criteria to ensure scalability, sustainability, and deployment of these impactful innovations; and 3) building a strong implementation plan for integrating it effectively across the entire ecosystem.
4. Treat innovation as a marathon, not as a sprint. How do we ensure our clinical quality work is running on a tech timeline? How do we use innovation bridge rails for the advancements of emerging technology to solve problems of our high-cost, low-value system? How can we stop shoehorning every digital solution into existing workflow infrastructure and call it “innovative” — but rather undercover the existing problems and solve them using the digital approach from our toolkit?
As Kyle Malady, chief technology officer at Verizon emphasized during the symposium, “Digital innovation is hard work… and the future won’t invent itself. Despite the daunting task that lies before us, fear not. This future-scape of digital healthcare delivery is an exciting one.” The only way forward is to be as brave as the people who need us.
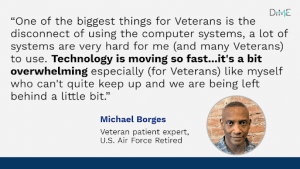
5. Technology doesn’t discriminate — and neither should our innovations. A digital-inclusion approach is essential to mitigate existing disparities created by the emerging digital technologies. Intentional efforts to narrow the digital divide should be reinforced in every team, culture and institute rather than leaving a section of the population technologically handicapped.

During the symposium, leading experts from Google, UnitedHealthcare Group, and Verizon also offered remarks underscoring the opportunity for VHA to lead digital health transformation across the entire nation.
Maintaining VHA’s Leadership in the Digital Era of Healthcare
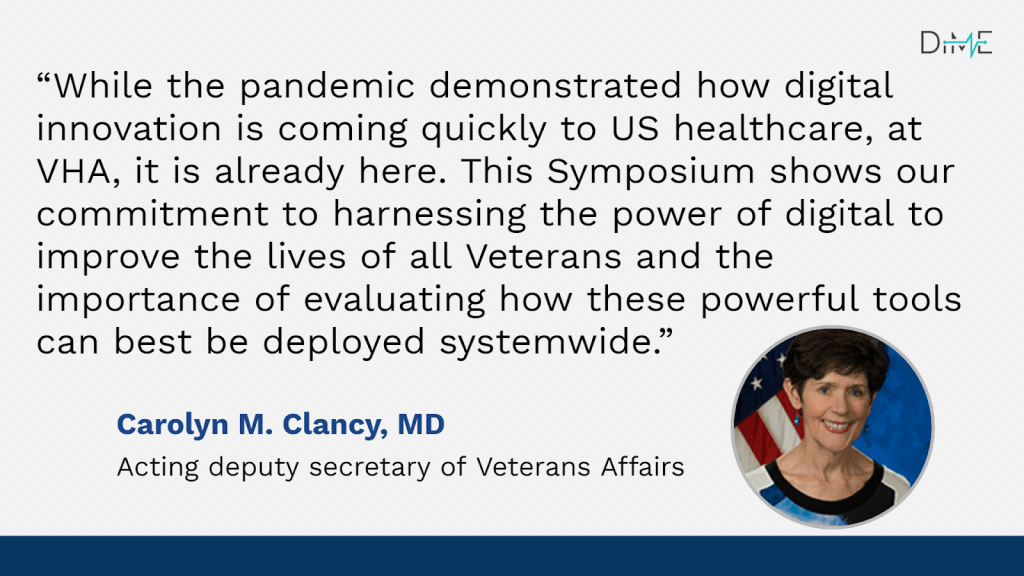
Though the COVID-19 pandemic showed, in dramatic ways, the advances in digital health, the foundation for the revolution we’re seeing has been building for years at the VHA. Dr. Clancy, acting deputy secretary of Veteran’s Affairs also emphasized that, “VHA has been at the digital revolution forefront, supporting and investing in digital health early on, particularly in the area of telehealth since 2003.”
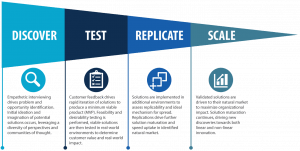
The VHA Innovation Ecosystem (VHA IE), has proven their innovative lead by successfully building an innovation model supporting the entire life cycle of innovation in the largest and highly complex integrated health system in the U.S.
DiMe-VHA’s Commitment to Advancing Digital Innovation
VHA IE is working to accelerate healthcare’s slow pace of digital transformation by addressing the lack of a standard model for operationalizing and scaling innovation. Together, VHA IE and DiMe are committed to developing a robust conceptual framework to measure and evaluate prospective digital health solutions to improve Veteran-centered care.
For a long time, the value of innovations has been measured through a return on investment model that we believe is disproportionally weighted toward cost savings rather than value creation. Evaluating innovation measures with such a narrow focus on financial returns has failed to meet the needs of individuals, systems, and society. There is a system-wide need for a shared understanding of how innovation can deliver value and how this may vary over time. This is particularly important during an unprecedented era of rapid innovation driven by digital solutions and the data flows and computing capabilities that underlie them.
Together, VHA IE and DiMe will create a strategic and sustainable roadmap for digital innovation across the VHA, specific digital implementation and quality improvement initiatives, and a toolkit of resources to support the deployment of the framework bolstering the successful digital transformation.
To support other health systems, innovators, industry partners or any decision makers in evaluating digital health innovation, VHA IE and DiMe envision sharing the innovation framework and the best practices with the whole U.S. healthcare system.
Join us to continue to push for the most innovative ways of turning our ideas into insights and transforming insights into innovative solutions at VHA to improve the lives of 9+ million Veterans across the nation and beyond:
- Read the full summary report of the VHA Digital health symposium
- If you would like to participate in the upcoming VHA-DiMe Industry symposium, register here
At DiMe, our commitment to fully integrating experts from all of the disciplines comprising digital medicine is unwavering. From regulators to white-hat hackers, ethicists to engineers, and clinicians to citizen scientists, we are proud to welcome all experts committed to ensuring that digital medicine realizes its full potential to improve human health. Join us!


